From the depths of the mind
How UF researchers have turned 3-D-printed dreams into research realities
By Morgan Sherburne, Alisha Kinman, Michelle Koidin Jaffee and Brittany
Across the campus of the University of Florida, researchers are taking 3-D printing into their labs and into their hands, using the technology to create a replica heart with a patient’s specific genetic defect, to explore a reproduction of a patient’s brain, to use a patient’s tumor for personalized medicine, and to print a brand new smile. Here are a few ways UF scientists are printing their way out of problems, both scientific and clinical.
From anemones to arteries
Steve Ghivizzani, Ph.D., and Tommy Angelini, Ph.D., along with other University of Florida researchers are working together to find medical applications for a type of 3D printing Angelini has developed.
Imagine printing a three-dimensional flap of skin to help heal people who have suffered from severe burns.
Imagine growing blood vessels to help feed that tissue.
Imagine building a section of kidney, brain or liver.
How about a tumor, printed from the cells of a malignancy inside a patient, that physicians could use to see how the cancer might respond to chemotherapy?
These are things physicians have considered for a long time, but haven’t had the technology to explore — until now, say researchers Steve Ghivizzani, Ph.D. and Tommy Angelini, Ph.D.
Angelini, a professor in the UF College of Engineering’s department of mechanical and aerospace engineering, studies the way cells move.
“The way we normally answer these kinds of questions is to study cells on flat, two-dimensional surfaces,” Angelini says. “We would watch a single cell crawl around on a surface, or create a uniform layer of cells, and watch the motion within that monolayer.”
But that single layer of cells doesn’t replicate how cells move or relate to each other in a three-dimensional structure, like they would in a living tissue. When cells are surrounded by other cells, they move differently, they receive nutrients differently and they grow differently. Angelini wondered how he could study the behavior of cells when they’re surrounded by other cells in three dimensions.
The answer was in a material composed of microscopic, granular particles called microgels. The material looks like a liquid, but acts like a solid. It will conform to the shape of any container it’s placed in, but will also hold materials that are placed within it, in the exact same position, indefinitely.
“One way to understand it — if you look at bottles of hand sanitizer at the grocery store, you can see air bubbles, or little colored beads, trapped in place,” Angelini says.
In this liquid-like solid material, Angelini has printed shapes of jellyfish, a hollow knotted rope, a series of vase-like shapes that look like Russian nesting dolls. He’s currently perfecting an anemone. When Angelini discovered that cells could survive in it, he knew the medium could be used in medical applications.
“Once I started working with the material, I realized this isn’t just a way to study fun questions about how cells behave — this is a 3-D printing method,” Angelini says. “That’s when we ran into Steve.”
At the UF College of Medicine’s annual Celebration of Research event in 2015, Angelini and fellow department of mechanical and aerospace engineering researcher Greg Sawyer, Ph.D., connected with Ghivizzani, who studies cell biology and leads the Gene Therapy Laboratory in the UF College of Medicine’s department of orthopaedics and rehabilitation.
Ghivizzani immediately saw the technology’s potential.
“A huge problem in biomedical research has been an inability to create cellular materials in the laboratory that have a blood supply,” Ghivizzani says. “When you do tissue engineering, and place that tissue into an animal, there’s no vasculature — the cells of that tissue quickly die.”
What if, he thought, they could print and grow tubular or vascular structures in the liquid-like solid, and then build tissues around them?
“It seems possible in theory, but the ability of this technology to produce complex tissues had never been tested,” Ghivizzani says. “So in talking with the guys about how to use this technology, I said, ‘Let’s start with something simple.’”
That simple thing? Tumors.
“When a tumor grows in an organism, it generates a simple three-dimensional structure.” Ghivizzani says. “As it grows, the cells within the tumor must constantly change their biology to adapt to the changes in their growth environment.”
Tumors often grow where other, healthy cells aren’t able to, and the blood vessels that grow around and within the rapidly expanding tumor are often deficient.
“Growth conditions often vary widely within individual tumors. Some regions will be nutrient rich, and other regions of the tumor are starved,” Ghivizzani says.
This makes the biology of the cancer cells that researchers study in labs — in those uniform two-dimensional sheets — much different from the cancer cells that grow in tumors within the body. The conditions in laboratory cultures are ideal for cell growth: All cells live in the same oxygen and nutrient-rich environment, and are under no stress. But how the same cancer cells behave in a body is a completely different story.
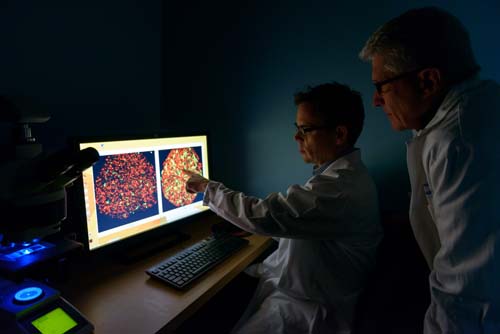
Ghivizzani with Angelini and Sawyer have been able to infuse the granular microgels with growth medium, and print thousands of tumors overnight. Having a multitude of tumors means not only can researchers study how tumors grow in three dimensions, they also study how tumors vascularize, compare the sensitivities of different tumors to chemotherapies, and quickly screen drug combinations to find those that have the best chance of eliminating the cancer, Ghivizzani said.
Printing tumors is a lot faster and less expensive than growing tumors in animal models — and animal models often don’t provide good replicas, as many human cancers don’t grow well in animals. These mini tumors can also be grown inexpensively, using cells from a patient’s own tumor.
Angelini’s jellyfish and anemones? They are delicate and beautiful — but they also teach the researchers how they may be able to print vasculature for tissue in the future.
“Cancer engineers its own growth and environment to form a tumor within the body. Hopefully, studying this process will provide us with a roadmap of how to use this technology, and teach us where we need to go. We just have to work to get there,” Ghivizzani says. “But it’s not something that’s only going to be available tomorrow. This is today stuff.” — Morgan Sherburne
Advanced imaging lies at the heart
Researchers analyze a patient’s heart scans to select data, which is then loaded onto a device called a 3-D slicer. The slicer segments areas of the body that physicians would like to print, and what results is a model of that patient’s heart, true to size.
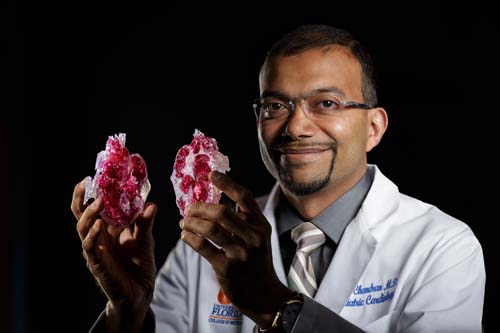
Arun Chandran, MBBS, FAAP, FACC, holds a pediatric patient’s heart in his hand and analyzes the twisted ventricles. Turning the organ, he examines a hole within the heart and the inverted ventricles that accompany it. But the heart that Chandran is holding is not real — in fact, it’s a 3-D-printed, full-sized model of a heart that is composed of hard resin.
Chandran, the director of the pediatric cardiac MRI/CT imaging program at the UF Health Congenital Heart Center, in conjunction with the UF biomedical engineering department, is using new technology to create models of their patients’ hearts in order to study abnormalities inside the heart before physicians decide how to treat the patient.
“Many of our 3-D-printed hearts are from children of all ages, including newborns. I convey to parents that by going through with this procedure our physicians are able to learn more about their child’s heart defect through a pain-free, noninvasive approach,” Chandran says. “We now have the ability to hold a heart in the palm of our hands without causing the child discomfort.”
The center has been at the forefront of pediatric cardiac magnetic resonance and computed tomography imaging for more than 10 years and has been creating volume-rendered 3-D images for the same duration. However, over the past six months, physicians at the UF Health Congenital Heart Center have extended their services to 3-D printing on patients who range from newborn to adulthood.
In June 2015, doctors started using this new procedure, which may change the way they image heart defects. In collaboration with John Forder, Ph.D., an associate professor of radiology in the UF College of Medicine, the UF Health Congenital Heart Center introduced 3-D printing of intracardiac anatomy, or the inside of patient’s hearts, based on CT data from patients with complex congenital heart disease.
Physicians scan patients’ hearts using computed tomography and MRI scans.
These scans recreate the patients’ hearts, defects and all, which the physicians can then print using 3-D technology. With the copies of patients’ hearts in their hands, physicians can better diagnose rare and complex heart defects and these models then provide their cardio-thoracic surgeons with as real a road-map as possible prior to actually performing the surgery on the child.
“EKG and echocardiograms continue to be the initial step of diagnostic imaging with any of our patients. However, with these new scanning technologies, our physicians are given more options to choose from when deciding on the next level of imaging they would like to pursue,” Chandran says.
Noninvasive techniques such as 3-D printing also reduce the risk of pain to patients and are more cost-effective.
For the past 10 years, the UF Health Congenital Heart Center has treated patients of all ages living with congenital heart and has made significant strides in pediatric cardiac imaging through the UF Health Pediatric Cardiac Magnetic Resonance/Computed Tomography Angiography Center of Excellence.
In 2005, the UF Health Congenital Heart Center became one of first centers in the nation to implement 64-slice computed tomography angiography, a machine that scans for congenital heart disease by taking quick photographs of the heart. In 2008, the center became one of first centers to use a 320-slice scanner for patients with congenital heart disease. The scanner provides better spatial resolution at faster speeds and, as a result, improves diagnostic accuracy while lowering a patient’s exposure to radiation.
“Unlike treating a patient for a common cold or a broken bone, the heart is a complex muscle where every patient case we see is unique,” Chandran says. “As a result, the needs of scanning for one patient can be very different from the other.” — Alisha Kinman
To train a neurosurgeon

On the ground floor of the Evelyn F. and William L. McKnight Brain Institute, two 3D printers churn out life-sized replicas of patients’ skulls and spines, offering unparalleled practice opportunities to today’s medical residents and even veteran surgeons.
On the ground floor of the Evelyn F. and William L. McKnight Brain Institute, two 3-D printers churn out life-sized replicas of patients’ skulls and spines, offering unparalleled practice opportunities to today’s medical residents and even veteran surgeons.
The models are a key part of a training simulator developed at UF that enables residents to learn and practice on specific patient anatomies without risk, time limits or pressure. The simulator also allows experienced surgeons the chance for a run-through before a complicated case.
Using uploaded MRI and CT scans, a UF Health lab prints replicas of patients’ anatomy made out of a fine, calcium-based powder similar to Plaster of Paris that is then dipped in a vat of super-strong glue. Residents then use a simulator of a fluoroscope, an X-ray device that enables surgeons to see the inner-workings on a computer screen as they insert and move a surgical probe inside a patient’s head.
“We built virtual fluoroscopy machines so we can simulate doing a lumber puncture, doing a surgery for trigeminal neuralgia or practicing complex spine surgery,” says Frank Bova, Ph.D., a medical physicist and director of the RadioSurgery/Biology Lab, who has led development of the virtual training experience.
In the past, plastic models did not include abnormal anatomies, Bova said. With the 3-D printer, exact replicas of patients are produced, giving residents the chance to learn techniques on a variety of realistic patient anatomies. With the virtual fluoroscopy machine, they learn to coordinate their hand movements with the images they see on the screen without exposure to actual X-rays.
A grant from the National Institutes of Health enabled development of the systems, and the first 3-D-printed model was sent to the operating room in 2007. Surgeons used it to understand the patient’s complex anatomy and determine how best to resect a tumor on the spine.
“With the model in hand, they were able to turn it around and look for planes where they could separate the tumor from the bone,” Bova says.
Researchers in Bova’s lab continually work to refine the materials to make sure they feel right. For example, when drilling through the skull, a surgeon receives tactile feedback at various intervals to understand when to stop drilling.
“We’ll have the practitioners come in and say, ‘Yep, that feels right,’ or ‘no, that’s too soft.’ Then we adjust the materials accordingly,” Bova says. “We can teach the residents so that when they touch the first patient, they have done this and they know what it feels like.”
Bova, who was named UF’s Inventor of the Year for 2013, and colleagues in the Lillian S. Wells Department of Neurosurgery use the models to allow students to struggle and make mistakes, in order to learn more effectively. Unlike real fluoroscopy, the virtual machine produces no radiation, so Bova can let the machine run, whereas it’s normally limited to a matter of seconds.
“It looks and feels real to them and it looks real on the screen, so I can let them work at it and then say, ‘Let me show you what you’re doing wrong’ and correct them,” Bova says.
With the cost of 3-D printers used in health care down to about $10,000 and dropping, treatments taking advantage of them are continuing to expand. Bova’s team has begun using 3-D printers in new ways, such as creating a piece of skull that fits a patient who has had to have a piece of his or her own skull removed.
“We print a mold of the bone and sterilize it. Then, in the operating room, we physically build a piece and hand it to the surgeon who then fixes it to the patient’s skull,” Bova says.
His team is also using 3-D printers to create masks custom-made for a patient’s face that serve as a guide system for surgeons. The masks have a straw-like protrusion where a probe can be inserted. By inserting the probe through the protruding piece, the surgeon is guided directly to the tumor or other target. This use could be particularly beneficial to hospitals lacking the resources of major medical centers, as the mask could be made at UF and shipped overnight to remote locations.
“I could 3-D print this and deliver it to Palatka, Florida, to Uganda, to any place in the world and someone could do very precise image-guided surgery for pennies now, because these things are really cheap to 3-D print,” Bova says.
While the masks are still in clinical trials, Bova expects them to be in widespread use within the decade.
“Relatively soon,” Bova says, “3-D printers will be inexpensive enough that a physician can have one on his or her desk.” — Michelle Koidin Jaffee
3-D printing a smile
Many patients at the UF College of Dentistry are getting 3-D printed smiles.
Dental implants, bridges and crowns are just a few of the things being produced with the help of 3-D printing, offering patients stunning smiles at a low cost and helping revolutionize dental manufacturing. Using X-rays and CT scans, 3-D printing software helps dentists and dental specialists to practice future surgeries and create guides for their patients’ planned surgeries.
William Martin, D.M.D., FACP, the director of the Center for Implant Dentistry and a prosthodontist in the department of oral and maxillofacial surgery, said his department uses 3-D printing for dental implant procedures, an additive manufacturing process that fabricates the surgical guides from scratch.
“We primarily use the 3-D printer to fabricate what we refer to as a template or surgical guide that is inserted into the mouth when we are placing dental implants,” he says. “They actually guide us in preparing the bone for positioning the dental implant ideally based upon a digital blueprint.”
Using special X-rays known as cone-beam CT scans, Martin said the clinic creates three-dimensional images that are imported into software where the treatment team can virtually perform the surgery.
“So we can perform the surgery in the computer before we execute it in the mouth,” Martin says.
Once the surgery is practiced on the computer and the dental implants are placed exactly where they need to be, a surgical template is designed that fits into the patient’s mouth at the time of surgery that will guide the surgeon in that exact direction, Martin said. That template design is then sent to the 3-D printer, which will print and fabricate the surgical guide so it can be inserted into the mouth during the implant surgery.
The 3-D printer makes the process go much smoother, allowing for increased accuracy and decreased surgical and healing time, Martin said. The printing technology also acts as a beneficial tool for making educational materials to train dentists, offering the same degree of accuracy and consistency to each item printed.
“The ability to print in combination with the software technology is really opening up avenues that we didn’t have before,” he says. “It shows the kind of technology we have, where we are going and the different things we can do.”
Similar to 3-D printing, computer-aided design can also be used for a subtractive process, known as 3-D milling — a process used by Geraldine Weinstein, D.D.S., a clinical associate professor at the UF College of Dentistry.
“Instead of building something from plastic or whatever you want to print with, we are taking away from a block of porcelain and cutting it into shape and size, like a crown for a tooth,” says Weinstein.
The process is completed with the help of large milling machines, but is still designed using the same process as that of 3-D printing. This method is used for restorations like crowns and bridges.
Not only does this allow the clinic to deliver these restorations at a lesser cost, the procedure can also take place in the same day.
“In years past, we used to have to send impressions of the tooth to the lab and have it made and have it come back two weeks later,” Weinstein says. “But now we get it the same day and we can provide the patient with the restoration immediately. Patients don’t have to wait — with uncomfortable temporary crowns — anymore.”
Dental students also reap some rewards from this 3-D technology. According to Weinstein, there are very few schools that teach their dental students these kinds of procedures in the clinical area.
“I think it is to our advantage that we have all the equipment here,” she says. “It adds to the prestige of the university and prepares our young dentists for the future.”
Although they have many differences, both of these printing processes are limited by the materials that are currently available for use.
“As we get more materials developed, there will be more options in types of restorations down the line,” Weinstein says.
Regardless, this technology has made its impact on dentistry and will continue to have a place within the industry, Martin said.
“If you were to say do you have a wish list of equipment that you want in your clinic, the 3-D printer would be in the top three of my wish list,” he says. — Brittany Valencic
